By Rita Brhel, managing editor and attachment parenting resource leader (API)
 Depression is beyond epidemic proportions, not only in the United States but in many societies around the world. People like to blame more recent economic downturns, but these high rates of depression have been an ongoing concern for many years from before the stock markets took a dive.
Depression is beyond epidemic proportions, not only in the United States but in many societies around the world. People like to blame more recent economic downturns, but these high rates of depression have been an ongoing concern for many years from before the stock markets took a dive.
If depression was the H1N1 Influenza virus (a.k.a. swine flu), no one would venture to the streets or grocery store without a face mask for fear of transmission, schools and businesses would be closed indefinitely, and medical clinics and hospital emergency rooms would be packed with people clamoring for screening and treatment.
But depression isn’t contagious like the flu – although it certainly is more debilitating and has just as much potential to kill. It doesn’t spread by sneezing and coughing, but it is still “contagious” in that people living with a depressed significant attachment figure, whether adult-adult or parent-child, are more likely to develop depression themselves and all that comes with this illness – the hopelessness, the sorrow or anger depending on the person’s response, the suicidal thoughts and possible attempts.
Depression is pervasive in the United States, and it is devastating to families – to marital relationships and to children’s development. We know through attachment research and neuroscience that the way we are parented not only affects the behavior we use in reaction to stressful events but also changes the way our brains work and our genes express brain chemistry reactions to stress. This means that if we are parented in such a way that consistently teaches us to react poorly to stress and conditions our brain to release stress chemicals at high rates, we are literally creating a child who will grow up into an adult who is prone to depression and all that comes with it.
Our families are in crisis.
New Report Brings to Light the Impact of Parental Depression
A new report, Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention, was released by the National Research Council and Institute of Medicine of the National Academies last week at a public briefing in Washington, D.C. Attachment Parenting International attended via webcast.
The National Academies consist of the National Academy of Sciences, the National Academy of Engineering, the Institute of Medicine, and the National Research Council. They are private, nonprofit institutes that provide science, technology, and health policy advice to the United States under a congressional charter.
Depression in Parents, Parenting, and Children explores the interaction of depressed parents and their parenting practices, and the impact on children. It also proposes strategies to promote more effective interventions, as well as recommendations for improving the quality of care for depressed parents and their children. The study was funded by the Annie E. Casey Foundation, The California Endowment, the Robert Wood Johnson Foundation, the U.S. Health Resources and Services Administration, and the U.S. Substance Abuse and Mental Health Services Administration.
Report committee members who attended the briefing included: Chair Mary Jane England, MD, president of Regis College in Weston, Massachusetts; William Beardslee, MD, professor of child psychiatry at Children’s Hospital in Boston, Massachusetts; Mareasa Isaacs, PhD, executive director of the National Alliance of Multi-Ethnic Behavioral Health Associations in Bethesda, Maryland; and Frank Putnam, MD, professor of pediatrics and psychiatry at the Cincinnati Children’s Hospital Medical Center in Cincinnati, Ohio.
The Prevalence of Depression
The briefing opened with an overview of depression in the United States, presented by Isaacs. The exact number of people affected with depression is difficult to pinpoint, but it’s estimated that only one-third of adults with the illness actually receive treatment. In some sample communities, as many as 70% of people with depression go without treatment. Although depression treatment is very effective, there are a number of factors preventing people from seeking help: the stigma of mental illness, lack of transportation, inability to afford services and medication, language and cultural barriers, and lack of providers or at least those with training in identifying and treating depression.
Despite not knowing the full extent of depression, there are several tendencies that Isaacs pointed out:
- Women have double the rate of depression as men.
- Caregivers are more likely to have depression.
- Depression typically first shows in adolescence or young adulthood.
- Those living in poverty are more likely to have depression.
- Depression is more common among adults who are separated or divorced than those who are married.
- Depression rarely appears alone – 75% of people who suffer from depression also suffer from traumatic histories such as sexual abuse or exposure to early childhood violence, substance abuse, a medical condition, or another mental health disorder especially anxiety or post-traumatic stress disorder.
- The development of depression rests in a combination of genetic susceptibility, environmental factors, and individual vulnerability. Depression is as much the result of other issues in a person’s life, as it is the indicator that there are additional problems.
- The majority of adults suffering from depression are parents.
The Impact of Parental Depression
It is this last point – that the majority of adults suffering from depression are parents – that is the take-home message. It is estimated that in the United States alone, one in five parents are affected by depression each year, or approximately 7.5 million. Here’s the kicker: 15.6 million children under age 18 live in these households where at least one parent is depressed, Isaacs said. Depending on the age of the child, they can be as much as 40% more likely to develop depression themselves with just one depressed parent in the home, said Putnam said – let alone both parents. “Mothers and fathers are often depressed together,” Beardslee added.
Remember what we know about attachment and how this affects the development of our children. For more than 15 million children in the United States, either their primary attachment figure or a strong secondary attachment figure is depressed and modeling all that comes with it.
“Depression is primarily a family issue,” Isaacs said. “It affects not only the individual but also children and other members of the family. It affects parenting.”
While the majority of research in parental depression has included mothers only, the few studies that have been conducted on fathers shows that the impact of children living with a depressed secondary attachment figure is just as devastating as living in a home with only the primary attachment figure suffering from depression, she said.
“Many people don’t get treatment, and those who do, don’t for years,” said Beardslee. “This makes a great impact on the family.”
Depressed parents tend to raise their children in an emotionally detached, withdrawn parenting style that affects the development of attachment, Putnam said. People with depression use fewer positive parenting approaches and more intrusive handling of children, and the end result is a child who is himself withdrawn.
“Depression causes terrible suffering,” in both parents and children, Beardslee said. Depression effectively destroys the attachment between a parent and child. The inconsistencies in parenting by depressed parents leads to a break in trust between the child and his parent. Long-standing depression causes neglect and often abuse. While depression symptoms manifest themselves differently in each person, women tend to be sad and withdrawn while men tend to be irritable and acting out.
Beardslee told of one mother who described what depression does to her parenting: When she isn’t depressed, she has very positive, emotionally close, and healthy interactions with her 12-year-old son, and when he comes home from school, they go through a routine of talking with, playing, and otherwise spending time with one another. But, when she is depressed, all that positive parenting disappears – she puts her son in front of the television and ignores the routine and his emotional and physical needs.
This break in routine, which is so important especially for older children, greatly affects the mental health of the child, Beardslee said. He feels inadequate, as though he is to be blamed for his mother’s withdrawal. Her depression affects his self esteem and models her poor responses to stress – significantly increasing the risk that he will eventually develop depression himself and unhealthy coping mechanisms expressed through social, behavioral, and other mental problems. He will feel the effects of chronic parental depression long after his mother’s depression is treated.
Not every parent with depression will inadvertently or deliberately cause harm to their children, but parental depression increases the risks for spillover consequences during critical periods of child and adolescent development.
“We’re very concerned about the impact on children,” Putnam said. While there is only a 2-4% risk of a small child developing depression when there is a depressed parent in the home, this risk jumps up to 20-40% in adolescents. “What also comes with this is the risk of substance abuse,” which is predominant among depressed individuals, Putnam added.
“To break the vicious circle of depression, we need to refocus our view of this illness through a broader lens that sees the whole family, not just the individual with depression,” England said. Beardslee added: “We need to think about people who are depressed as parents first, and individuals with depression second.”
This goes beyond postpartum maternal and infant depression – the screening and treatment of which is becoming increasingly more commonplace in the medical care community: “The first few years of life are crucial, but we need to look more into the long term,” Beardslee said.
The Report Committee’s Recommended Solution
Currently, most screening and treatment of depression happens in primary medical care settings, Beardslee said. However, because depression is more typical in families living in poverty and perhaps without the means to see a doctor, there must be more avenues for depressed parents to find help. Because depressed parents are often withdrawn and difficult to engage, more types of service providers outside the mental health system need to be trained to spot the symptoms of depression and to direct those who need help to accessible entries into the health care system.
Once parents seek treatment, the mental health care system must change the way it treats this illness. Because of the impact on children, interventions should adopt a two-generational approach – parent and child – to effectively treat depression in families, Beardslee said.
Putnam listed these critical components to an effective model of family-centered treatment for depression:
- Integrative – meaning that all factors contributing toward the depression must be identified, whether this includes poverty, marital issues, health problems, etc.
- Comprehensive – meaning that all co-occurring conditions must be identified and addressed, such as substance abuse and anxiety disorders.
- Multi-generational – which encompasses screening and treatment for both parents and children by one mental health care provider rather than by separate providers who often don’t know the full extent of depression on the family members.
- Preventive – which includes teaching parents positive parenting skills and skills to cope better with stress.
- Developmentally appropriate – any treatment should appropriate to the particular age group of the children involved.
- Accessible – screening should be available through programs frequently used by at-risk families such as home visitation, Headstart and other school-based programs, federal nutrition programs, etc., and those parents who are identified as depressed should then be assisted in navigating the mental health system to receive treatment. In addition, the financial barriers of at-risk families must be addressed – many may not have insurance or income, and those who are able to afford services may have difficulty paying for services for more than one person in the family. Also, the mental health system must look into ways of delivering services in nontraditional settings to be able to reach at-risk families, including schools, prisons, community programs, and even homes.
- Culturally sensitive – which includes techniques to overcome language barriers, stigmas, etc.
“There are a number of exciting initiatives with parts of these features, but no program yet has all of these features,” Putnam said. As it is now, “parents with depression are like orphans” in the mental health system, he added.
To jump-start this model, Putnam suggested the mental health system focus first on implementing a two-generational, more comprehensive focus. More health care providers need to receive training specifically in multi-generational depression. Practices should look into ways that would reduce the financial impact on at-risk families such as charging on a sliding scale, combining children and parent charges into one office visit instead of two, and negotiating with insurance companies to provide same-day reimbursements on medical care services. Once programs are in place that effectively treat family depression, they should be included in training models for other providers.
In addition, more research dollars need to be allocated toward studies that look at the impact of parental depression on children as well as the differences between the impact of depression in fathers and mothers, Putnam said.
The report committee said this report represents a call for urgency from the U.S. Surgeon General and the various mental health organizations and agencies – a major mental health concern that needs to have a working plan in place in the next six to eight months.
What is API Doing?
API actively helps parents who are prone to depression or are depressed by teaching parenting skills and providing resources to help parents develop better ways of coping with stress and strong emotions. According to researchers at the University of Michigan, who reviewed the numerous studies on the subject, there is a link between social support and wellness. Support networks are vital not only in preventing depression but also in its treatment. Local API Support Groups provide parents with a way to develop a solid support system that can follow them through their child’s many developmental stages and the challenges that come with them.
And if parents do fall into depression, API Leaders can help direct parents to the treatment they need as well as continue providing support through the local group or personal consultations, free of charge.
Discuss this topic with other API members and parents. Get advice for your parenting challenges, and share your tips with others on the API Forum.
Neighbor: “Oh, your children are always so wonderful to be around! I can tell that you take parenting seriously.”
 The birth of a child is one of the most significant events in the lives of families. It is considered a rite of passage by many women and involves the first interaction between parents and their baby. There is much buzz today about the necessity of making birth a “family-centered” experience, where the focus is often on creating a special environment for bonding between parents and child in the first moments and days of life. But what if you are one of the women who experiences your baby’s birth as a Cesarean section? Is it possible to make your surgical experience into a family-centered birth?
The birth of a child is one of the most significant events in the lives of families. It is considered a rite of passage by many women and involves the first interaction between parents and their baby. There is much buzz today about the necessity of making birth a “family-centered” experience, where the focus is often on creating a special environment for bonding between parents and child in the first moments and days of life. But what if you are one of the women who experiences your baby’s birth as a Cesarean section? Is it possible to make your surgical experience into a family-centered birth? Family-centered birth is used to describe a birth that is more family oriented, allowing the new family to experience their birth more fully. Many believe that this cannot apply to a surgical procedure. This is not true. Even with a Cesarean surgery, you can have a family-centered birth if you know your options and choose to apply them. Some of the options will be the same as for a vaginal birth. You may have to work harder to have a family-centered birth in the event of surgery, but planning ahead — even if you don’t foresee a Cesarean — can go a long way. Make a birth plan! They won’t know what is important to you unless you let them know, and a birth plan is actually a legal contract as it is providing your wishes in a document provided to your birth team.
Family-centered birth is used to describe a birth that is more family oriented, allowing the new family to experience their birth more fully. Many believe that this cannot apply to a surgical procedure. This is not true. Even with a Cesarean surgery, you can have a family-centered birth if you know your options and choose to apply them. Some of the options will be the same as for a vaginal birth. You may have to work harder to have a family-centered birth in the event of surgery, but planning ahead — even if you don’t foresee a Cesarean — can go a long way. Make a birth plan! They won’t know what is important to you unless you let them know, and a birth plan is actually a legal contract as it is providing your wishes in a document provided to your birth team. Depression is beyond epidemic proportions, not only in the United States but in many societies around the world. People like to blame more recent economic downturns, but these high rates of depression have been an ongoing concern for many years from before the stock markets took a dive.
Depression is beyond epidemic proportions, not only in the United States but in many societies around the world. People like to blame more recent economic downturns, but these high rates of depression have been an ongoing concern for many years from before the stock markets took a dive.
 One of the biggest mistakes that new parents make is giving up too soon on soft carriers. Because we often do not have real-life models, wearing our babies can initially feel awkward. Babywearing is a learned skill that takes patience, and the best way to become an expert at wearing your baby is to wear your baby often. To help you do that, here are some general tips:
One of the biggest mistakes that new parents make is giving up too soon on soft carriers. Because we often do not have real-life models, wearing our babies can initially feel awkward. Babywearing is a learned skill that takes patience, and the best way to become an expert at wearing your baby is to wear your baby often. To help you do that, here are some general tips: My dear crying baby,
My dear crying baby, Parenting during the teenage years is as trying on the young adult as it is on his parents. But if your child was adopted or if you’re fostering, the teenage years can be an especially tough time as your child tries to sort out his identity without knowing his birth parents or understanding the reasons why his birth parents are not a bigger part of his life.
Parenting during the teenage years is as trying on the young adult as it is on his parents. But if your child was adopted or if you’re fostering, the teenage years can be an especially tough time as your child tries to sort out his identity without knowing his birth parents or understanding the reasons why his birth parents are not a bigger part of his life.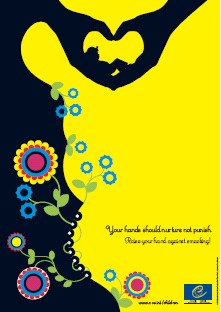 The Council of Europe wants a continent free of corporal punishment. Hitting people is wrong — and children are people, too.
The Council of Europe wants a continent free of corporal punishment. Hitting people is wrong — and children are people, too. We now have a multitude of studies that show mothers and babies should be together, skin-to-skin (baby naked, not wrapped in a blanket), the baby’s neck extended slightly so his head is in “sniffing position,” immediately after birth – and they should spend as much time together skin-to-skin as possible in the days that follow. The baby is happier, the baby’s temperature is more stable and more normal, the baby’s heart and breathing rates are more stable and normal, and the baby’s blood sugar levels are better.
We now have a multitude of studies that show mothers and babies should be together, skin-to-skin (baby naked, not wrapped in a blanket), the baby’s neck extended slightly so his head is in “sniffing position,” immediately after birth – and they should spend as much time together skin-to-skin as possible in the days that follow. The baby is happier, the baby’s temperature is more stable and more normal, the baby’s heart and breathing rates are more stable and normal, and the baby’s blood sugar levels are better.